Oculoplasty Services
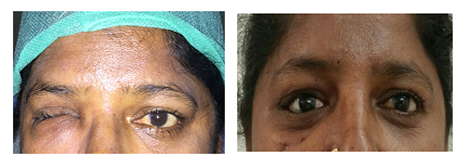
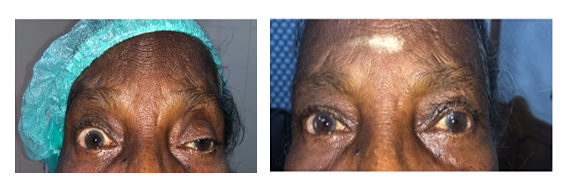
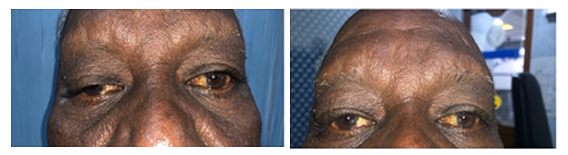
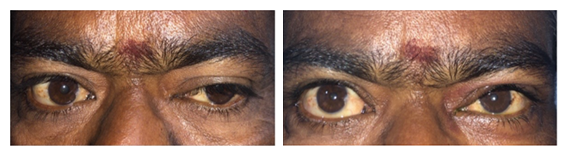
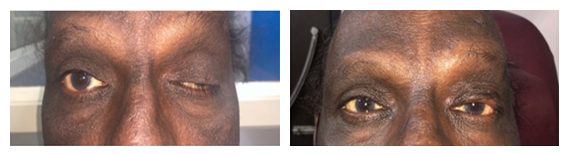
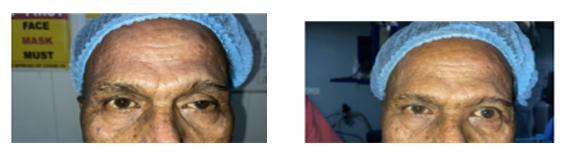
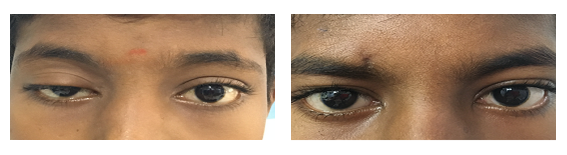
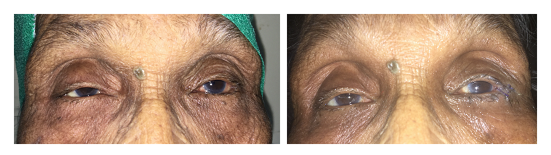
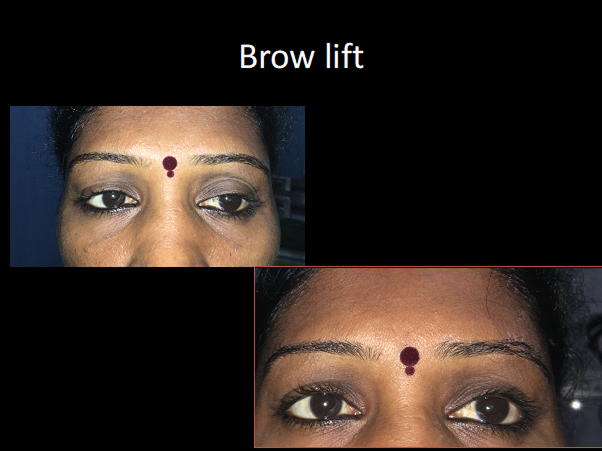
Droopy eyelid (ptosis) can occur as a result of birth defect, injury, muscle disorder, nerve disorder, recurrent allergy, contact lens use or simply due to aging. It gives a sleepy appearance, and can even obstruct vision if severe.
Ptosis may also cause excessive forehead wrinkling, abnormal head posture such as chin elevation, and eye fatigue. In children below 8 years of age, droopy eyelid can affect vision leading to a lazy eye (amblyopia). In adults, droopy eyelid is mainly a cosmetic concern. Surgery can correct this problem by repairing the muscle that lifts the eyelid.
There are various treatment options which include scarless approach, anterior approach reattaching the muscle responsible for elevation and lifting the lid with a sling. Ptosis surgery is a day care procedure. The procedure is simple and gives complete satisfaction most of the time. 5 -10 % may require second stage revisions as all muscles do not react same always

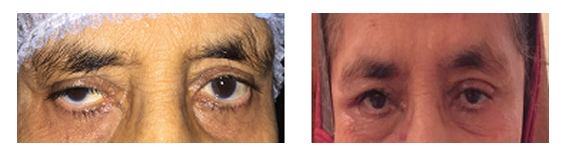
Inward turning of the lid is called entropion. This causes profuse watering and erosion in the cornea due to constant rubbing. This can lead to corneal ulcers which can decrease the vision. We correct entropion by simple surgeries which are day care procedures.
Ectropion is a condition in which there is outward turning of the lid. It can occur due to aging and laxity of tissues. Ectropion causes profuse watering due to constant exposure of the eyes.
Nasolacrimal duct is the drainage pathway of tears. Tears are secreted by lacrimal glands and are then drained via the puncta and they reach the nasal cavity. When there is a block in the nasolacrimal duct then there is constant watering and discharge from the eyes. This mechanical block can only be cured by doing a surgical connection between the sac and the nasal mucosa bypassing the block.
Patients with profound block tend to develop acute dacryocystitis which is a very painful condition. There is diffuse swelling of the eye with blurring of vision. This condition can be successfully corrected by a surgical procedure called the dacryocystorhinostomy (DCR). It can be done via the external approach or in the internal approach. Internal approach is being done with the help of endoscopes.

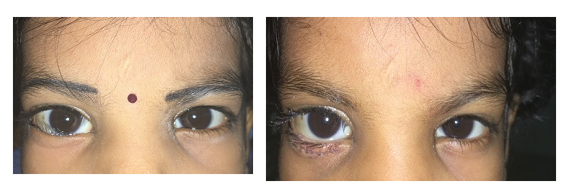
Lid mass can be cosmetically be a simple benign cyst to more aggressive malignancy. Early intervention will be life saving and cosmetically appealing. The procedures are usually done meticulously without any scars.
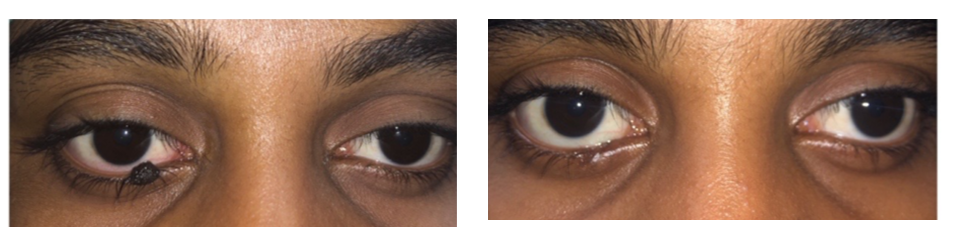
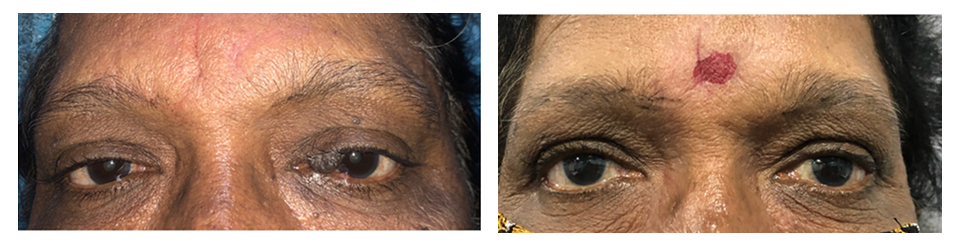
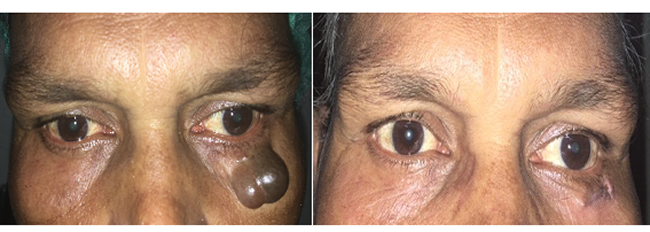
Figure 1 and 2 showing the malignant tumour in right eye lower lid

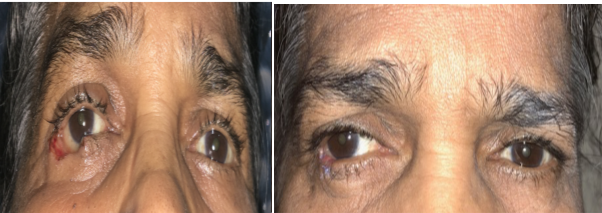
Figure 3 shows lower lid after excision of the mass

Figure 4 right eye after lid reconstruction

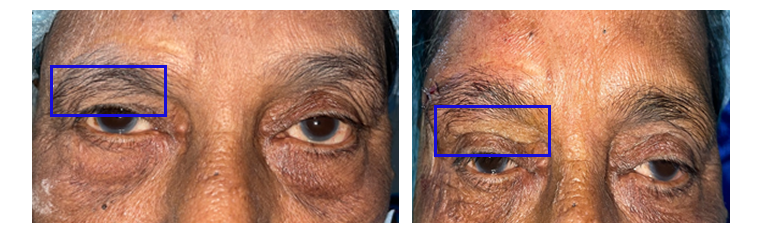
Fractures in the orbit can occur from trivial fall injury or major Road traffic accidents. Fracture in the orbit can cause double vision, defective vision and enophthalmos(eye appearing small).
Orbital fractures can be corrected with mesh, implants and titanium implants based on the size of the fracture. The implants can be customized to give better cosmetic appearance.
Figure 1 has fracture left eye with enophthalmos fig 2 is 1 week post op of left eye status post fracture correction with medpore implant



An ocular prosthesis is placed in the eye socket of people who have lost their eyes due to trauma, infection and tumours. A prosthetic eye can help improve the appearance of people who have lost an eye due to injury or disease. It's commonly called an artificial eye." It's not really an eye, but a shell that covers the structures in the eye socket.
A prosthetic eye can improve the appearance of the affected eye socket. If the entire eye is removed, an ocular implant and prosthesis gives a better cosmesis.
Many patients succumb to dreadful corneal diseases and unforeseen emergencies every day. After removal of the natural eye and placement of a prosthetic eye, a person will have no vision in that eye but it will boost up their self confidence and give them lot of moral support.